

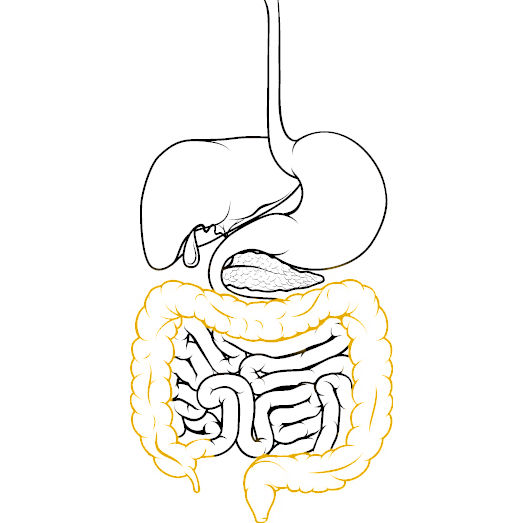
A colonoscopy is a test to examine the lining of the large intestine (also called the colon or large bowel). It is a safe procedure which provides information that other tests may not be able to.
Colonoscopy is often used as a screening test to check for polyps or cancer in the colon. A polyp is an abnormal growth in the colon which might turn into a cancer if it is left untreated. If we find polyps during colonoscopy, they can be safely removed to reduce your risk of developing colon cancer. Colonoscopy is also used to investigate for causes of symptoms (see below).
Most guidelines recommend colon cancer screening from age 45. If you have a strong family history of colon cancer, or certain other medical conditions, you may benefit from commencing screening at a younger age.
You might need a colonoscopy if you have:
• Blood in your bowel motions
• A change in your bowel habit
• A low blood count (anaemia) from iron deficiency
• Abdominal or rectal pain
• Previously had colon cancer or colonic polyps
We will provide you with detailed information about what to do before a colonoscopy. Specifically which foods to eat and which to avoid, and which medications to stop taking.
The colon needs to be cleaned out prior to a colonoscopy. We will give you bowel prep, a special drink that causes you to have watery diarrhoea. It is important to drink all of it to make sure your colon is clean. Having a clean colon allows us to have a more detailed, higher quality examination of the lining of the colon.
You will be given medications through an intravenous line (a needle placed in a vein in the hand or arm) to make you feel relaxed and help you to sleep through the procedure. The medication will be given by an Anaesthetist who will be monitoring your vital signs (blood pressure, heart rate, oxygen saturations and level consciousness) throughout.
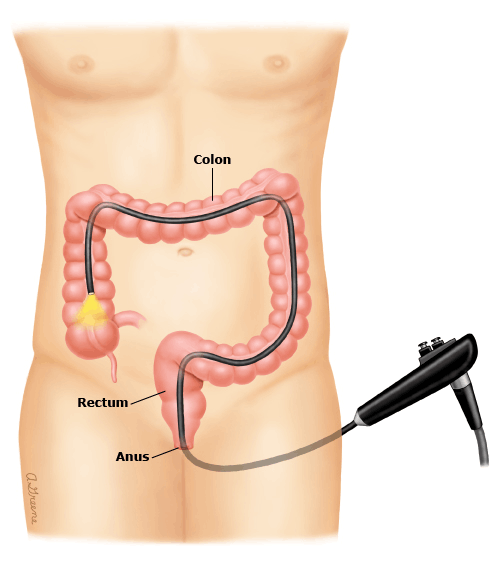
The endoscopist will gently pass a thin tube with a tiny camera and light on the end into your anus (bottom) and steer it to the start of the colon.
During the procedure, we might might take a small sample of tissue from your colon (a biopsy) to be examined under a microscope. If polyps are found at colonoscopy they are removed during the procedure. The lining of the colon is not pain-sensitive so you will not feel it if biopsies are taken or polyps are removed.
After the colonoscopy, you will be monitored for 1 to 2 hours in the recovery area until the anaesthetic medicines wear off. You will be given something to eat and drink. We will see you in recovery and discuss with you the findings of the procedure and the next steps.
You won’t be able to drive for the rest of the day after your procedure, so it is important to have someone who can pick you up and take you home. If this is not possible, let us know in advance and we can arrange alternatives for you. Most people can drive and go back to work the following day.
We will tell you when to start taking any medicines we asked you to stop before the test.
Colonoscopy is a safe procedure, and complications are rare but can occur:
• Bleeding can occur from biopsies or the removal of polyps, but it is usually minimal and can be controlled.
• The colonoscope can cause a tear or hole in the colon. This is a serious problem that sometimes requires surgery to repair, but is a very rare complication.




Copyright TES 2024